Using the SESG to Bolster Staffing Challenges for RTs
An SESG panel discussion with Garry Kauffman, Lenny Nyangwara, and Laura Quinn.
Getting Started
While the Introduction can help RT leaders get started, a full subscription to the SESG serves as a complete set of Activity Time Standards, resources, references, and tools to support staffing programs for a broad range of respiratory services. Each concept in the Introduction is included in greater detail through the subscription version of the SESG. In addition, SESG methodology, resources, and tools can be applied in a variety of clinical services, even nursing based departments, in which staffing is driven by clinical activities/procedures.
A real challenge is convincing decision-makers, administration, consultants, and even RT staff that using SESG methodology and time/value-weighted metrics is the most effective approach to staffing respiratory services. For that reason, the SESG includes not only the Activity Time Standards, but other content intended to support the application of systems and methodologies described. The content and structure of the SESG is easily accessed through a member exclusive website designed with intuitive access, navigation, viewing, and select downloads of content and tools.
Tips to get started once you have subscribed to the SESG:
- Get familiar with the content.
- Identify the challenges that may have prevented you from implementing an effective staffing program and use SESG content to gain a better understanding of key concepts before crucial discussions with stakeholders.
- Identify all clinical and support activities and apply the SESG methodology to develop your time standards and validate them using the SESG statistical tables.
- If you already have time standard-based metrics, use the SESG statistical tables and methods to validate existing time standards.
- Use the Excel workbooks to get started and modify the workbooks for your specific set of procedures and practice.
- If facing challenges and looking for ways to enhance your services and value, check out the specialized chapters on CPT codes, case studies, informatics, CPGs, “Making the Case,” and Value Efficiency.
- Lastly, take advantage of the Annotated Bibliography, the AARConnect SESG Community, and ongoing education and updates provided through the AARC.
- If you like what you see in the Introduction, please purchase to the SESG.
How the Information in the SESG Assists You to Manage Your Labor Resources
The SESG identifies clinical activities commonly performed and provides statistically validated time standards for each activity. RC leaders can use time standards to determine labor hours required by applying procedure counts to these time standards. These metrics can be incorporated into existing department systems and hospital information systems, or by using the pre-configured Labor Efficiency Worksheets provided in the SESG.
SESG reported activity times also assume that an RT is performing only one activity at a time. Performing multiple activities simultaneously diminishes the time spent with individual patients, reduces the quality of the service, does not allow for ongoing observed assessment of the patient, and actually brings into question whether an RT is required to deliver a service.
The SESG not only serves as a tool to track trends and changes in the number of staff needed with changes in workload, but also the impact of new programs and the introduction of new equipment, supplies, or clinical policy/protocols. By applying the time required in the provision of clinical services and the hourly cost of practitioners, estimates of direct variable clinical labor cost can also be determined.
The SESG will assist RT leaders to ensure an appropriate match of resources and demands by helping to answer some key questions, such as:
- What is the efficiency/productivity of staff, individually, within a patient care unit, per shift, and in the department?
- What are the number of Full-Time Equivalents (FTEs) needed to safely and efficiently perform respiratory care patient services and support activities?
- What will be the impact of new technology on hours required to deliver care?
- What full-time/part-time staff mix is most efficient based on variability in work demand?
- What will be the impact on resources of using CPGs, protocols, and policy changes to reduce misallocation?
- How many FTEs are required to implement a new service?
- What would be the reduction of FTEs resulting from discontinuing a service?
- What common set of characteristics should be captured in the process of benchmarking for best practice and labor productivity?
- How can I validate our own internally developed procedure time standards?
- How much time and expenses are consumed in care that has no medical indication or no value?
- What should be included in a comprehensive staffing plan?
Using the SESG to Establish a Productivity Reporting System
Measuring and reporting the productivity of staff is assessed through determining the time required to provide services in relation to the hours worked by staff who are providing those services. The Activity Time Standards contained in the SESG provide the mechanisms to determine the time required to deliver clinical services.
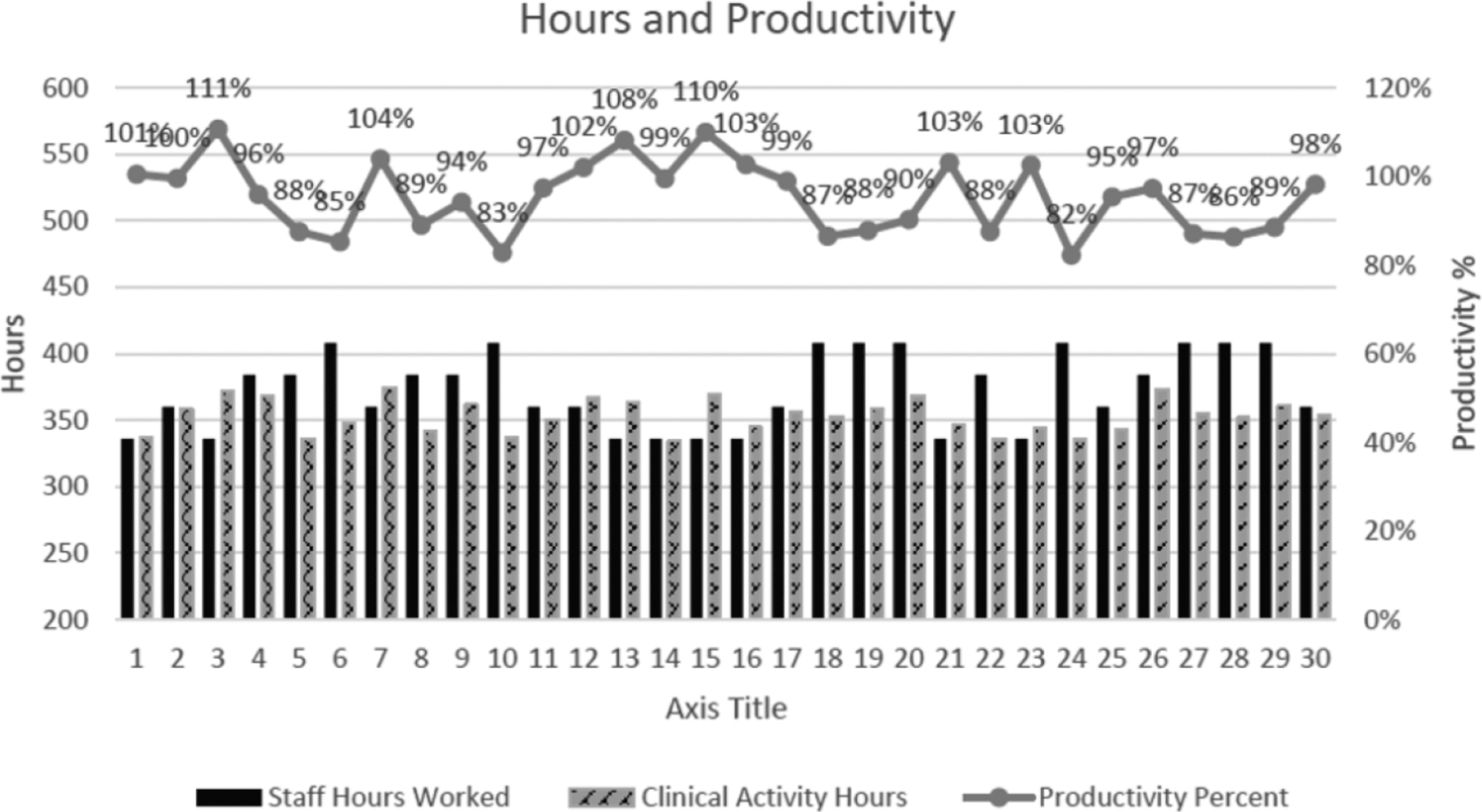
Productivity is derived from the relationship between the staff hours worked to provide clinical services and the Clinical Activity Hours required. The graph in Figure 2.1 provides one example of how productivity may be reported using SESG methodology.
There are several key concepts that should also be considered in the assessment and determination of productivity that are further explained in the SESG. These concepts include:
- Understanding fixed vs. variable labor hours and activities.
- Identifying clinical activities with time standards.
- Identifying clinical activities without time standards.
- Accounting for support activities.
- Accounting for non-allocated activities.
Fixed Vs. Variable Hours and Activities
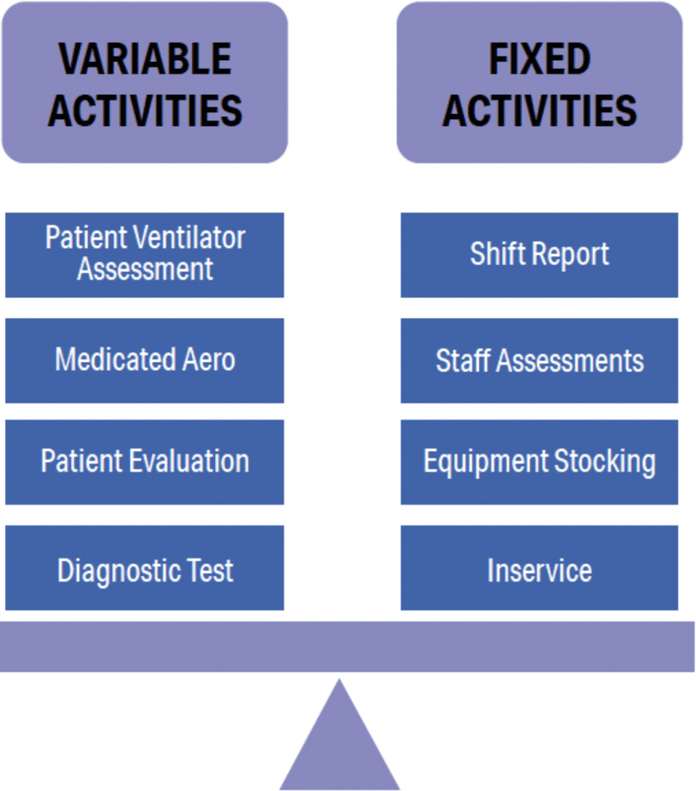
Whether labor hours are classified as fixed or variable can be determined by answering a simple question: Does the number of labor hours required to perform an activity change with changes in activity volume?
If labor hours vary directly with the volume of activities/procedures performed, those labor hours are classified as variable hours. These are typically bedside clinical activities.
If labor hours do not vary directly with the volume of service performed, then the associated labor hours are considered fixed. An example of fixed labor is time spent by supervisory personnel performing next shift workload assessment, patient care assignments, and other operational tasks.
Labor hours are allocated or justified using both the number of clinical activities as well as time for fixed activities. When determining productivity, the total of all fixed and variable activities must be determined.
In addition to understanding what hours and activities are fixed or variable, it is also important to understand the 3 components of the time required to deliver patient care.
Activities can be classified into the categories identified in figures 2.2 and 2.3:
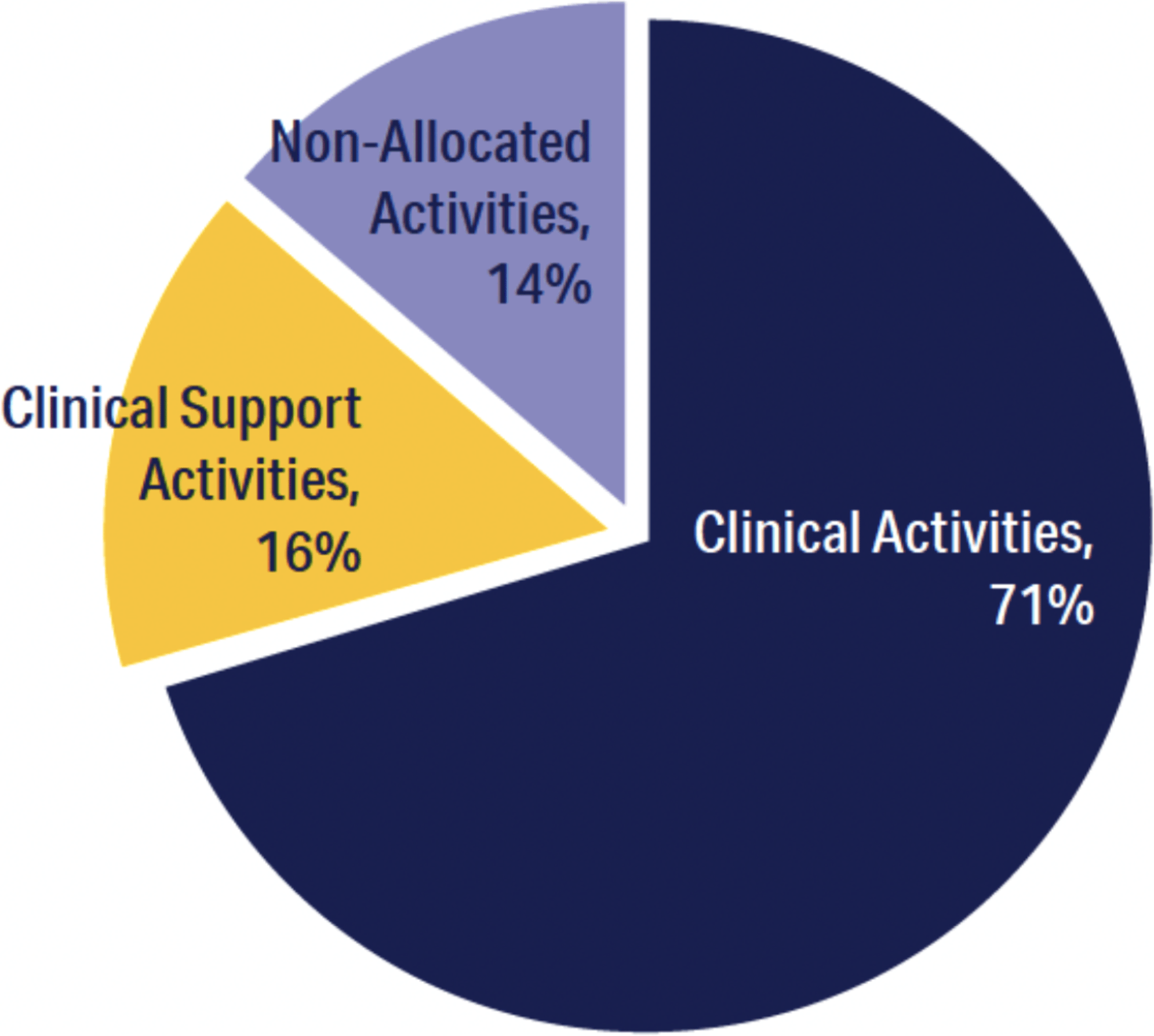
Definition of Clinical Activities
Clinical activities represent direct care/treatment/support to patients. These activities are requested to be performed through physician orders or medical staff approved respiratory care protocols. The Expert Team updated the activity definitions that were included in the 2025 SESG Time Standard Survey and the grouping of each activity into the below service groups. Inclusion of these activities in the SESG was then dependent on statistical analysis qualifying the activity for inclusion. In the SESG, each of these activities includes an activity definition and the time standard metrics of central tendency derived through data submission of RC leaders.
- Acute Respiratory Care Activities (64 Activities)
- Echo and Non-Invasive Cardiovascular Diagnostic Activities (40 Activities)
- Tests and Procedures Related to the Analysis of Blood Gases and Electrolytes (25 Activities)
- Tests and Procedures to Assist in the Diagnosis of Pulmonary Disease (62 Activities)
- Diagnosis and Treatment of Sleep Disorders (12 Activities)
- Hyperbaric Oxygen and Wound Care (9 Activities)
- Pulmonary Rehabilitation (40 Activities)
It is important to note that not all your clinical activities applicable to your facility may have a time standard included in the SESG. There are three reasons why:
- In the expert team review of the primary scope of practice they did not include all procedures that could be performed by respiratory care staff.
- There was not adequate statistical significance in the survey data for a specific procedure to qualify as a valid and reportable time standard.
- In surveying department managers for User Defined Activities, it was not reported to be performed.
In such cases users are referred to the SESG chapters on Methodology to Determine Activity Time Standards. Users are highly encouraged to use such methodology to identify new time standards and in refining SESG time standards to accommodate their specific situation.
Definition of Clinical Support Activities
These are activities performed to support the delivery of clinical activities. They may or may not require direct patient interaction. Major categories of these activities include:
- Management of equipment and supply activities associated with equipment acquisition, cleaning, storage, preventive maintenance, and distribution.
- Management, supervision, and staff support activities, including department administration and management, staff education and training, administration of quality systems, and information management.
- Preparing physical space for care or testing. Includes equipment quality assurance, calibration, testing, and equipment disinfection.
Depending on the nature of support activities, some are considered fixed while some are variable.
Definition of Non-Allocated Time
Non-allocated time in most cases is not directly associated with the provision of clinical or support activities. Non-allocated time varies depending on department/facility policy and practice. These activities include staff time required for shift change; travel time between care units; communication with other health care providers, patients, or families; meals; and paid breaks.
Example: During a 12-hour shift, the type of non-allocated and support activities could include 30 minutes for shift report, 15 minutes for unit travel, 15 minutes for stocking, 30 minutes for paid lunch, and 2 mandated 15 minute breaks.
In this case, 2 hours of time in a 12-hour shift is spent in non-allocated and support activity. The determination of labor hours required and the reporting of productivity must acknowledge that only 10 hours are actually available to perform clinical activities in a 12-hour shift.
Defining Worked Hours Available to Perform Clinical Activities
Worked hours must be accounted for to determine total productivity. However, not all worked hours can be spent in performing procedures or direct variable activities and described as support or non-allocated time. The example below demonstrates that in an 8-hour shift only 6 hours are available to provide patient care. Your numbers may vary, and subscribers can utilize the SESG workbooks to determine clinical time available:
| Total Worked Hours | 8.0 |
| Subtract Time Spent in Report | 1.0 |
| Subtract Paid Breaks per Shift | 0.5 |
| Subtract Transit Time | 0.5 |
| Time Available for Clinical Activities | 6.0 |
This simple example demonstrates the misconception that 100% of worked hours are available to perform direct patient care. Expecting RTs to provide patient care for all worked hours is not feasible and may be a concern with regard to safe and effective provision of care.
In addition, the concept that all paid hours do not account for worked hours available for clinical care is another factor that must be considered. How many paid hours are actually worked includes determination of factors including paid vacation, paid sick leave, and paid holidays.
Determination of how many Paid Hours can be worked and how many of those Worked hours can be spent in performing direct patient care are factors that must be considered in reporting actual productivity.
Making the Case, Getting Decision Makers On-Board
You may understand the value of the SESG, but how do you engage your leadership to adopt? The SESG contains several important tools, documents, and resources that will strengthen your knowledge about productivity and staffing and help you communicate the value of what the SESG can offer.
The chapter “Productivity Systems — The Importance of Accurate Time Standards” will help you understand the issues related to a variety of metrics to determine staff hours required, inclusive of billable procedures, procedure counts, patient days and the benefits of using activity time standards and other weighted systems. The AARC position paper titled “Best Practices in Respiratory Care Productivity and Staffing” is a valuable resource that can help you communicate with and educate your leadership. These documents and a wealth of others are found in the SESG Educational Resources and the Annotated Bibliography. Lasty the case studies will provide a unique insight into the success and benefits experienced by real users of the SESG.
As discussed, while the SESG provides nationally reported procedure time standards, it is important to understand there are reasons why your procedure times may vary. These include:
- The expert team review of the primary scope of practice did not include all procedures that could be performed by respiratory care staff.
- The survey data did not include adequate statistical significance for a specific procedure to qualify it as a valid and reportable time standard.
- In surveying department managers for User Defined Activities, the procedure was not reported to be performed.
In identifying why your time standards may differ from the SESG, consider the following:
- Procedures common to all activities differ.
- Charting and your EMR may demand more or less time to complete.
- Procedures and protocols that dictate steps and tasks associated with the procedure differ.
- Physical space inclusive of the location of department/ supplies, unit layout, elevators, etc.
For these reasons, every facility should determine if any of the SESG procedure time standards need to be modified to align with practices in their department (see Methodology for Developing Time Standards). In cases where there are significant differences between any of your facility-specific procedure times and the SESG, you have the opportunity to ensure decision-makers understand the reasons why you may take longer in performing a procedure.
Clinical Activities with Time Standards
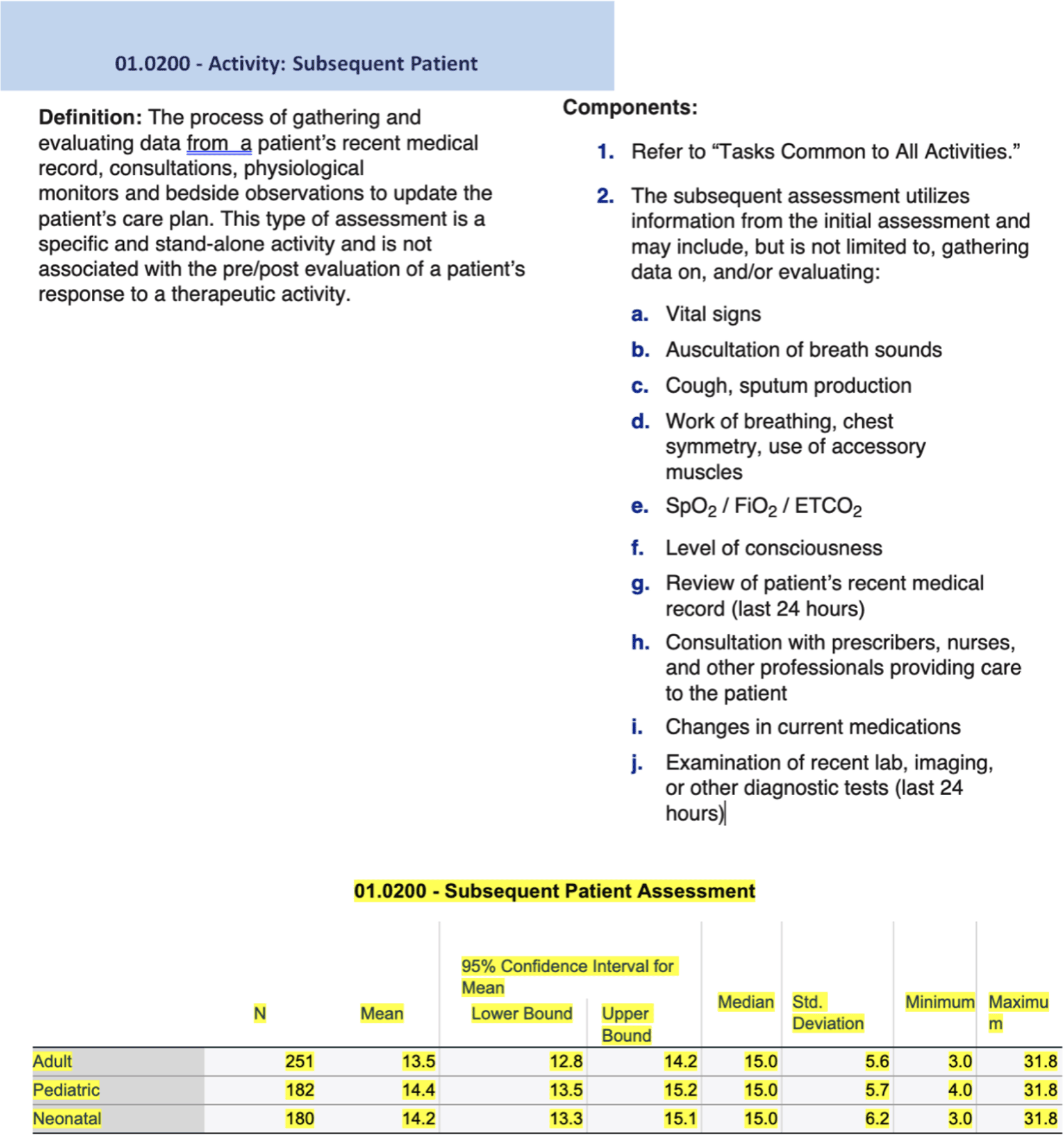
The long-standing hallmark of the AARC Uniform Reporting Manual and the 2020 rebranding of what is now the SESG, has been the inclusion of Clinical Activities Time Standards. The SESG includes procedure definitions and time standards as a result of a national survey and appropriate statistical methodology to validate times reported via this national survey or RT leaders. There are over 250 activity times reported in the 2025 SESG. The examples below for “Initial Patient Assessment” and “Subsequent Patient Assessment” are utilized to provide readers of the Introduction with an understanding of what is included in the SESG:
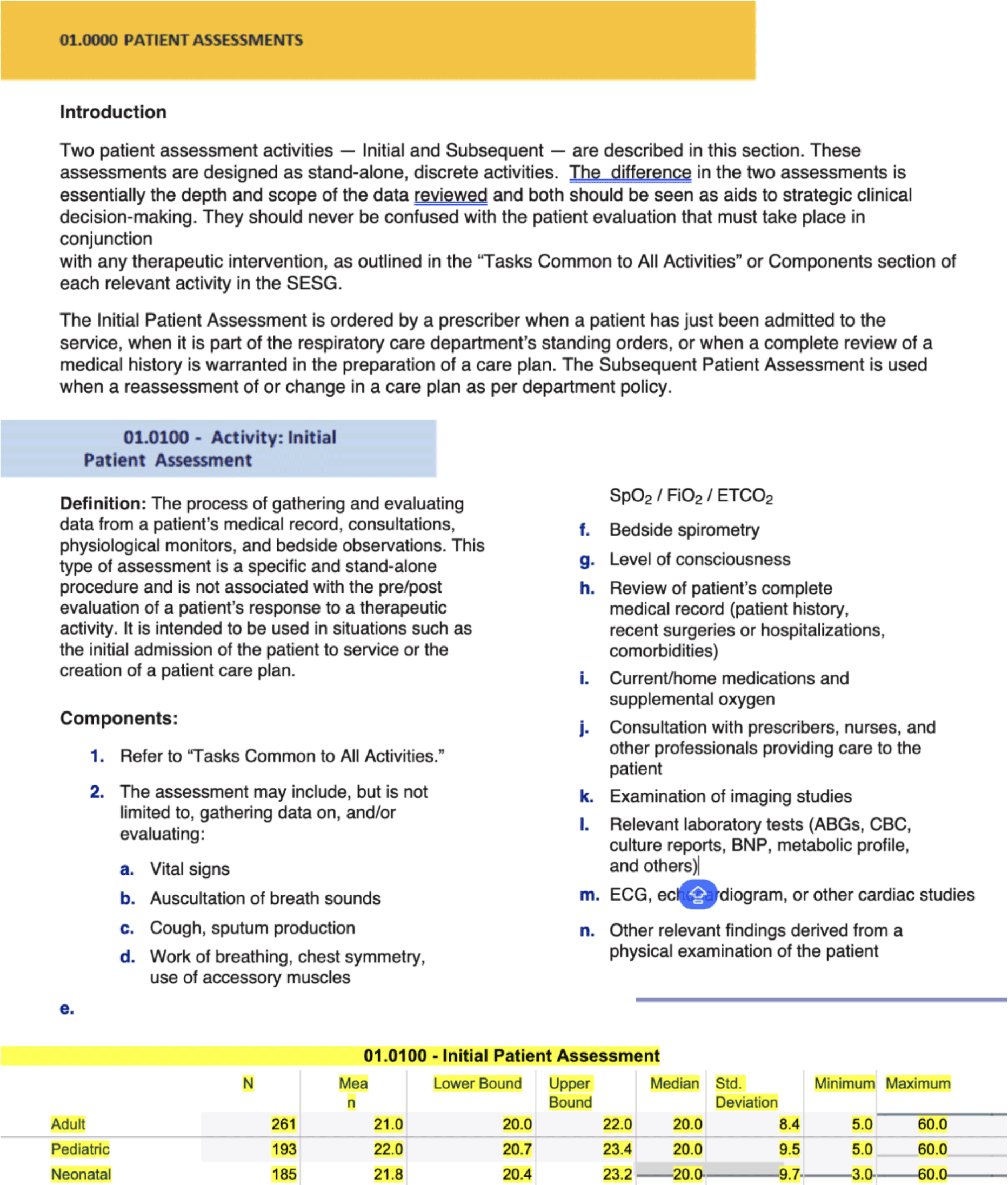
Other Activities that Support the Delivery of Respiratory Care Services
It is critically important to account for the time spent in activities that support the delivery of clinical services when determining staff productivity. The approach to accounting for this time can range from reporting and including specific or groups of support activities for which time standards have been developed to defining a standard percentage of working hours that typically account for all patient support activities. Remember, total time worked consists of these components:
- Time spent in delivering clinical services
- Time required to conduct the activities to support the delivery of those clinical services
- Non-allocated time
- Fixed activities
Fixed Activities
Many of the activities supporting the provision of direct patient care services or fulfilling administrative responsibilities are often referred to as “fixed activities” because the resources required do not vary directly with the volume of services. Shift reports and department meetings are examples of fixed support activities.
A characteristic of fixed activities is that they do not vary significantly with the workload and can therefore be identified as a specified number of hours for each reporting period. For example, 30-minute shift report at shift start and shift end total one hour per shift of fixed time for each RT.
Although fixed activities do not vary significantly with workload, they can vary based on other factors, such as the number of staff, the number of shifts worked, clinical units assigned, or use of a specific piece of equipment. Such relationships need to be defined and incorporated into the department productivity management system.
Support Activities
It may make sense to treat some support activities as a variable rather than fixed if the labor hours spent in the support activity directly vary with the volume of clinical activities performed. For example, if calibration of a device is required after a certain number of uses, the frequency of the calibration activity will be driven by the number of times the device is used rather than the time it is in service.
In this instance, the time standard would also be calculated by using the “average time” formula described in the introduction to the “Statistical Methodology for Developing Time Standards.”
Extremely Variable Clinical and Support Activities
Some activities occur infrequently or require extremely variable amounts of time, thus making it impossible to determine a validated standard time. An example of this is preparation for a visit from an accreditation agency that may occur only once in several years. Activities like these may be accounted for by using an “actual time.”
Some Support and Clinical Activities, such as Transports, may require highly variable amounts of time, depending on the patient’s acuity, technology that must accompany the patient, the location, and the reason for the transport. In such situations the department may want to capture actual time or use a time interval unit, such as 15 minutes, in which case a 45-minute transport would be counted as three 15-minute increments. Such methods of capturing actual time can be applied in determining demand or assigning work.
Identifying Support Activities
The following steps will assist you in developing a comprehensive list of applicable support activities:
- Identify all activities of the workday that meet the definition of “support activities.”
- Validate by engaging your staff to review.
- Refine the list to combine those activities that are similar as well as eliminate those activities that occur infrequently.
If desired, establish time standards for selected tasks or groups of activities. Refer to the document titled, “Statistical Methodology for Developing a Time Standards” to establish these standards.
Additional Important Considerations
- If two therapists are involved in performing a clinical activity as a medical necessity, the time allocated for that activity should account for the total time of both practitioners.
- Be sure to educate, engage, and obtain approval from your administrative and medical leadership in the planning and implementation of your staffing plan and productivity systems. Engaging key stakeholders is critical to having your productivity model accepted as the standard for determining clinical staff complement.
- The brief definitions of clinical procedures provided in this Guide are not complete procedure descriptions. Rather, they provide guidance in helping the user define the activity applicable to the assigned time standard. RT leaders are encouraged to define each procedure/service to a level of detail that all RT staff fully understand and consistently apply.
- Accuracy in capturing procedure counts and calculating time standards, and vigilance in monitoring consistent application of these standards, will result in a uniform reporting system tailored to your service that is a useful management tool. This also applies to the inaccuracies in defining productivity that result by electing to use non-weighted and/or billable procedures that assign a ‘1’ to each procedure regardless of the time required. External consultants suggesting a “normalization” process to address this should be educated as to the lack of validation of this process. See the “RVU Considerations” chapter for additional information regarding use of billable procedures as well as actual experiences encountered.
- While accuracy in procedure capture is key in determining productivity, there are situations in which departments may not have systems in place to capture all the types of procedures listed in the SESG. In such cases users can consider combining a set of procedures that are common to the course of treatment. An example may be the inability to individually capture the set of SESG procedures associated with ventilator care. SESG procedures related to ventilator care include patient ventilator assessment, setting change, suctioning, parameter change, trach care etc. The 2025 version of the SESG also includes a new time standard for a Patient Day. Lastly, managers can focus on the 20% of activities that make up 80% of labor needed, identifying the top 10 or 20 activities that primarily drive staffing. Several facilities have taken this approach when it comes to work assignments.
While procedure time-based systems remain important in determining the number of staff required and justifying labor resources, one cannot ignore that value is even more important. Few would disagree that despite having a productivity system in place, there is nothing productive in consuming labor hours in the performance of procedures that are not clinically indicated for a particular patient or have little or no medical value. Patient focused respiratory care protocols (“protocols”) are one way to help ensure only medically indicated therapy is provided. Having both the SESG and protocol systems in place makes for a much more viable system to justify staff. In such cases the manager can then make the case with administration that a medically required procedure is ordered by the physician (or driven by protocols) and thus the hospital is expected to provide the resources to perform procedures and services approved by the medical staff. Further, the inability to provide resources as determined through SESG methodology places the patient and the institution at risk. For additional information on applying value as a key element in determining labor resources required, see the Value Efficiency Section of the Guide.
Next Steps
While the Introduction is intended to get you started in developing data and value driven staffing plans, you can obtain the complete AARC Safe and Effective Staffing Guide through the American Association for Respiratory Care. Your subscription will include the following and will also include updates over the course of the subscription period:
- Clinical Activity Definitions and Validated Time Standards
- Support Activities and How to Account for Them
- Methodology for Development of the SESG
- Methodology for Development of Time Standards
- Data Interpretation Guidelines
- Importance of Time Standards
- Case Studies in Productivity
- Informatics
- Making the Case: Getting Your Administrative Leadership on Board
- AARC Value Efficiency Position Statement
- AARC Value Efficiency Position Paper
- AARC Clinical Practice Guidelines
- AARC Position Statement on Unattended Procedures
- User Created Activities
- CPT Code Table
- CPT Code SESG
- Staffing Plan Template
- Annotated/Linked Bibliography
- Excel Productivity Worksheets Pre-Configured with Median Time Standards
- Ongoing Updates and Educational Programming
